Retinal detachment is a separation of the retina from its attachments to its underlying tissue within the eye. Most retinal detachments are a result of a retinal break, hole, or tear. These retinal breaks may occur when the vitreous gel pulls loose or separates from its attachment to the retina, usually in the peripheral parts of the retina. The vitreous is a clear gel that fills 2/3 of the inside of the eye and occupies the space in front of the retina. As the vitreous gel pulls loose, it will sometimes exert traction on the retina, and if the retina is weak, the retina will tear. Most retinal breaks are not a result of injury. Retinal tears are sometimes accompanied by bleeding if a retinal blood vessel is included in the tear.
Once the retina is torn, liquid from the vitreous gel can then pass through the tear and accumulate behind the retina. The build-up of fluid behind the retina is what separates (detaches) the retina from the back of the eye. As more of the liquid vitreous collects behind the retina, the extent of the retinal detachment can progress and involve the entire retina, leading to a total retinal detachment. A retinal detachment almost always affects only one eye. The second eye, however, must be checked thoroughly for any signs of predisposing factors that may lead to detachment in the future.
Flashing lights and floaters may be the initial symptoms of a retinal detachment or of a retinal tear that precedes the detachment itself. The symptoms of flashing lights and floaters may often be unassociated with a tear or detachment and can merely result from a separation of the vitreous gel from the retina. Cataract surgery, especially if the operation has complications, increases the risk of a retinal detachment.
Causes:
A loss of peripheral vision can follow a peripheral retinal detachment due to a tear or a hole. Most such cases will progress to a full retinal detachment and loss of all vision if the problem is not repaired. Spontaneous or self reattachment of the retina is rare.
Procedure:
Treatment
Retinal holes or tears can be treated with laser therapy or cryotherapy (freezing) to prevent their progression to a full-scale detachment. Many factors determine which holes or tears need to be treated. These factors include the type and location of the defects, whether pulling on the retina (traction) or bleeding is involved, and the presence of any of the other risk factors discussed above. Three types of eye surgery are done for actual retinal detachment: scleral buckling, pneumatic retinopexy, and vitrectomy.
Scleral buckling
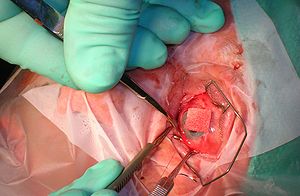
The surgery is done in an operating room with general or local anesthesia. In most cases it is done as an outpatient procedure. An indirect ophthalmoscope or operating microscope is used to identify the holes or tears. The hole or tear is then sealed, either with diathermy (an electric current which heats tissue), a cryoprobe (freezing), or a laser. The resulting scar tissue later forming around the retinal tear helps keep it permanently sealed, so that fluid no longer can pass through and behind the retina. A scleral buckle, which is made of silicone, plastic, or sponge, is then sewn to the outer wall of the eye.
Pneumatic retinopexy
Pneumatic retinopexy is a newer method for repairing retinal detachments. It usually is performed on an outpatient basis under local anesthesia. Again, laser or cryotherapy is used to seal the hole or tear. The surgeon then injects a gas bubble directly inside the vitreous cavity of the eye to push the detached retina against the back outer wall of the eye. The gas bubble initially expands and then disappears over two to six weeks. Proper positioning of the head in the postoperative time period is crucial for success. Although this treatment is inappropriate for the repair of many retinal detachments, it is simpler and much less costly than scleral buckling. Furthermore, if pneumatic retinopexy is unsuccessful, scleral buckling still can be performed. Vitrectomy
Certain complicated or severe retinal detachments may require a more complicated operation called a vitrectomy. These detachments include those that are caused by the growth of abnormal blood vessels on the retina or in the vitreous, as occurs in advanced diabetes. Vitrectomy also is used with giant retinal tears, vitreous hemorrhage (blood in the vitreous cavity that obscures the surgeon's view of the retina), extensive tractional retinal detachments (pulling from scar tissue), membranes (extra tissue) on the retina, or severe infections in the eye (endophthalmitis). Vitrectomy surgery is performed in the hospital under general or local anesthesia. Small openings are made through the sclera to allow positioning of a fiberoptic light, a cutting source (specialized scissors), and a delicate forceps. The vitreous gel of the eye is removed and replaced with a gas to refill the eye and reposition the retina. The gas eventually is absorbed and is replaced by the eye's own natural fluid. A scleral buckle is usually also performed with the vitrectomy.
Recovery tips:
Discomfort, watering, redness, swelling, and itching of the affected eye are all common and may persist for some time after the operation. These symptoms are usually treated with eye drops. Blurred vision may last for many months, and new glasses may need to be prescribed, especially because the scleral buckle may have changed the shape of the eye. The surgical repair of retinal detachments is successful in about 80% of patients with a single procedure. With additional surgery, over 90% of retinas are reattached successfully. Several months may pass, however, before vision returns to its final level.
About Eye
Eye Diseases
Vision problems
Find Cost
Surgeries & Treatments
Best Eye Hospitals
Testimonials
Get Free Quotes
Top Hospitals In India
Top Hospitals In Turkey
Top Hospitals In Mexico
Top Hospitals In Costa Rica
Top Hospitals In Singapore
Top Hospitals In UAE
Top Hospitals In Australia
Top Hospitals In Malaysia
Top Hospitals In Thailand
Top Hospitals In Phillipines
Cataract Surgery
Intacs
Astigmatic Keratotomy(AK)
Canalicular Tear Repair
Chalazion Surgery
Conductive Keratoplasty(CK)
Corneal Transplantation
Lasik Surgery